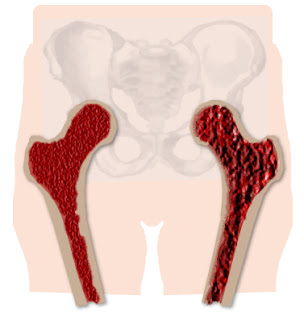
Osteoporosis usually is not detected until clear clinical symptoms such as reduced height and fractures. These usually occur in the thoracic and lumbar, neck, femur and distal radius.
Being an asymptomatic disease to presenting their bone complications need an early diagnosis, which is induced by clinical history, with analysis of genetic, nutritional, environmental and risk factors, and the determination of biochemical markers of bone age and bone mineral content measured by densitometry.
First you need a physical examination should include measurement of height to detect loss. Also useful are the x-profile of the lumbar and thoracic spine for the presence of vertebral fractures. To detect osteoporosis before symptoms appear can be measured bone mineral density (bone mineral density / BMD) by densitometry.
Currently, the two easiest ways to diagnose this disease:
1 º) using a dual energy radiographic densitometry (DEXA) of lumbar spine and hip, which quantifies the mineral content per unit area, so you get the bone mineral density (BMD) in g. cm2, relative to the projection area, and
2 °) by means of computed tomography (CT) that provides a bulk density in g. m3.
In 1994, a committee of experts from the World Health Organization proposed the densitometry criteria for diagnosis of osteoporosis in female population the values of mineral content or bone mineral density that fall below -2.5 standard deviations of the mean healthy young women (peak bone mass).
The diagnosis of osteoporosis can often go unnoticed if not think about it, because that is so insidious onset and lack of sensitivity of conventional diagnostic methods. Bone demineralization is not detected until they lose at least 30% of bone mineral density.
The fracture is the result of osteoporosis. We think of it so that it can diagnose, but it would be very interesting if we could predict its occurrence, and this is very difficult to get, because there is different bone mass, depending on the mechanical factors that concur in the individual.
With noninvasive methods such as densitometry using ultrasound measurements can be made in patients who have a risk of osteoporosis, and when in doubt densitometry should be performed by dual X-ray absorptiometry to confirm the suspicion of osteopenia, an inexpensive and noninvasive way to predict this condition.
Patients exposed to prolonged treatment with glucocorticoids have a reduced bone mineral density, and 30-50% of them suffer vertebral fractures. The degree of bone loss is related to the duration of treatment and the dosage used. However the treatment as well as diagnose probably not related to the underlying diagnosis, age, or sex of the patient. The subjects with glucocorticoid-induced osteoporosis should be periodic monitoring of bone mineral density when they are on chronic steroid every 6 or 12 months.
Ideally we should have a baseline densitometry before starting treatment and then follow up every 6 months.
The use of biochemical markers of bone formation and restoration is a good step forward for diagnosis and treatment of osteoporosis. It seems that high values of these biochemical markers indicate a high bone remodeling and are associated with decreased bone mass.
They also serve to predict an accelerated rate of bone loss.
In osteoporosis, bone biopsy may be useful to study bone architecture and evaluate the decrease in trabecular interconnection or to evaluate the effect of treatment. However, bone biopsy is not essential for the diagnosis of osteoporosis because it can be done by the other methods we have discussed.
Popular Posts
-
Fish Oil Supplements For Osteoporosis Overview Imagine a sneeze causing a bone fracture. This is a possible scenario if you suffer fro...
-
Calcium , Osteoporosis , Hypertension And Colorectal Cancer Summary The results of epidemiological studies on the relationship between d...
-
How To Deal With Back Pain Back pain is an all-too-familiar problem that can range from a dull, constant ache to a sudden, sharp pain t...
-
Diet to Fight Osteoporosis The relationship between diet and health is beyond doubt. A balanced diet that includes all kinds of food as...
-
Osteopenia : Natural Remedies For Pre-Osteoporosis pre-osteoporosis Osteopenia is a pre-osteoporosis state characterized by a Reducti...
-
What Is Osteoporosis - Definition of Osteoporosis Osteoporosis is a condition characterized by mass (weight) and low bone damag...
-
What is Post Menopausal Osteoporosis? After 50 years, particularly in white women of small stature, there is a decrease in trabecular bone ...
-
Osteoporosis Vitamins Osteoporosis Treatment Methods Osteoporosis Treatment Osteoporosis is a condition in which the density i...
-
Osteoporosis Osteoporosis affects more than 28 million men and women in the United States. The often called "brittle bone disease...